Select Radiation Quantity
This converter works within each category (activity, exposure, absorbed dose, equivalent dose). Cross-category questions like “Bq to Gy” require extra physical context – see the explanation in the Formula section.
Enter Value & Units
Result
Converted: –
Scientific: –
Grouped: –
⏳ Radioactivity Decay Calculator (Half-Life)
Compute how activity changes over time using the exponential decay law. Units for activity (Bq, kBq, MBq, Ci) are handled by the same multiplier.
Decay Result
Remaining activity A(t): –
Fraction remaining: –
Fraction decayed: –
📏 MU ↔ Dose Helper (Machine-Specific)
For linear accelerators calibrated at reference conditions, dose is often approximately proportional to monitor units (MU). Enter your own calibration – this helper does not replace treatment planning.
⚠️ Clinical safety: Always verify MU with your department’s TPS / QA procedures. This helper is for educational use only.
Quickly match “what the number measures” to the right unit family
Need to convert a report in mSv, rad, rem, or Ci into SI units without mixing categories? The key is identifying whether your value describes activity, exposure in air, absorbed dose, or equivalent/effective dose—then converting only inside that family.
Last Verified: December 2025
- Activity (Bq, kBq, MBq, GBq, Ci): how many decays happen per second.
- Exposure (R, C/kg): ionization produced in air (legacy survey-meter style units).
- Absorbed dose (Gy, rad): energy deposited per kilogram of material.
- Equivalent/effective dose (Sv, rem): dose adjusted for biological effect (used for limits and comparisons).
Looking for similar pages? Browse the Unit Converters hub or use the Scientific Notation Converter for very large/small outputs.
Unit family map (what converts cleanly, with exact factors)
Everything below is a straight multiplier. If your question crosses rows (example: “Bq to Gy”), you’re no longer doing a unit conversion—you’re doing a physics/modeling problem.
| Quantity | Base SI unit | Common legacy unit | Exact/standard relationship | What it does NOT tell you |
|---|---|---|---|---|
| Activity | Bq | Ci | 1 Ci = 3.7×10^10 Bq | How much dose a person receives |
| Exposure (in air) | C/kg | R | 1 R ≈ 2.58×10^-4 C/kg | Dose in tissue without assumptions |
| Absorbed dose | Gy | rad | 1 rad = 0.01 Gy (100 rad = 1 Gy) | Biological effect (risk) |
| Equivalent/effective dose | Sv | rem | 1 rem = 0.01 Sv (100 rem = 1 Sv) | Where the dose was absorbed |
Prefix cheatsheet (where most “off by 1,000” mistakes happen)
Real-world reports often use prefixes (m, µ, k, M, G). The converter is correct, but interpreting the magnitude is where people slip.
| Unit | Prefix | Meaning | Example |
|---|---|---|---|
| Sv | mSv | 10^-3 Sv | 5 mSv = 0.005 Sv |
| Sv | µSv | 10^-6 Sv | 500 µSv = 0.0005 Sv |
| Gy | mGy | 10^-3 Gy | 2 mGy = 0.002 Gy |
| Bq | MBq | 10^6 Bq | 250 MBq = 2.5×10^8 Bq |
| Bq | GBq | 10^9 Bq | 3 GBq = 3×10^9 Bq |
Common math/logic mistakes (tool-specific)
- mGy vs mSv: Gy is energy absorbed; Sv is “effect-weighted.” They are not interchangeable numbers unless you state radiation type and weighting.
- µSv vs mSv: 1 mSv = 1,000 µSv. Mixing these changes the story completely.
- Ci vs mCi: 1 Ci = 1,000 mCi. A label in mCi is three orders smaller than a Ci value.
- “R to Sv” shortcuts: Any single-factor conversion hides assumptions about energy spectrum, geometry, and tissue.
Method used by the converter (simple, transparent multipliers)
Each mode converts your input to a base SI unit, then to the target unit. That’s why results are linear and reversible inside the same family.
Step 1: value_SI = value_input × factor_from Step 2: value_target = value_SI ÷ factor_to
Exact/standard relationships used here
Activity: 1 Ci = 3.7×10^10 Bq 1 Bq = 1 decay/s Exposure (air): 1 R ≈ 2.58×10^-4 C/kg Absorbed dose: 1 Gy = 1 J/kg 1 rad = 0.01 Gy Equivalent dose: 1 Sv = 100 rem 1 rem = 0.01 Sv
Why “Bq to Gy” is not a unit conversion
Activity (Bq) counts decays per second, but absorbed dose (Gy) depends on how much energy ends up deposited in a specific mass over a specific time.
To estimate dose from activity you typically need emission energy, exposure duration, distance/geometry, shielding, and the absorbing material/tissue. That is why this page keeps modes separate.
Worked examples (with short interpretations)
Example 1: Convert 2 mSv into Sv for a report
mSv means “millisievert,” so 2 mSv = 0.002 Sv. If your form is in Sv, entering 0.002 keeps the meaning unchanged.
Example 2: Convert 100 rad into Gy from an older document
1 rad = 0.01 Gy, so 100 rad = 1 Gy. This is a clean absorbed-dose conversion and does not imply biological effect by itself.
Example 3: Convert 1 mCi into Bq for activity labeling
1 mCi = 0.001 Ci, and 1 Ci = 3.7×10^10 Bq, so 1 mCi = 3.7×10^7 Bq (37,000,000 Bq).
Example 4: Convert 0.2 R into C/kg
Using 1 R ≈ 2.58×10^-4 C/kg, 0.2 R ≈ 5.16×10^-5 C/kg. Interpreting that as Sv requires additional context (energy/type and geometry).
Half-life decay calculator (how to read the output)
If you track activity over time, the important quantity is the number of half-lives elapsed: t / T1/2. Two half-lives means 25% remains, three half-lives means 12.5% remains.
A(t) = A0 × (1/2)^(t / T1/2)
Typical mistake
- Unit mismatch: entering half-life in days and elapsed time in hours without converting mentally can make the decay look “too fast” or “too slow.” The calculator converts units for you, but your expectation should match the chosen units.
MU ↔ dose helper (what the number means)
Monitor Units (MU) are machine-specific. Converting MU to dose only makes sense if you use your site’s calibration (for example, cGy per MU at reference conditions).
For engineering/physics utilities beyond this page, see Data & Computing tools and Energy & Environment tools.
Putting “mSv” in context (high-level ranges, not medical advice)
People usually ask “is this big or small?” for mSv values. A practical way to read a number is to compare orders of magnitude (µSv vs mSv) and consider whether it’s a one-time value or cumulative over time.
Educational note: imaging doses and risks depend on protocol, patient size, and scanner settings. Use your clinician/physicist for decision-making.
📈 Radiation Dose & Units – Visual Comparison (Infographic)
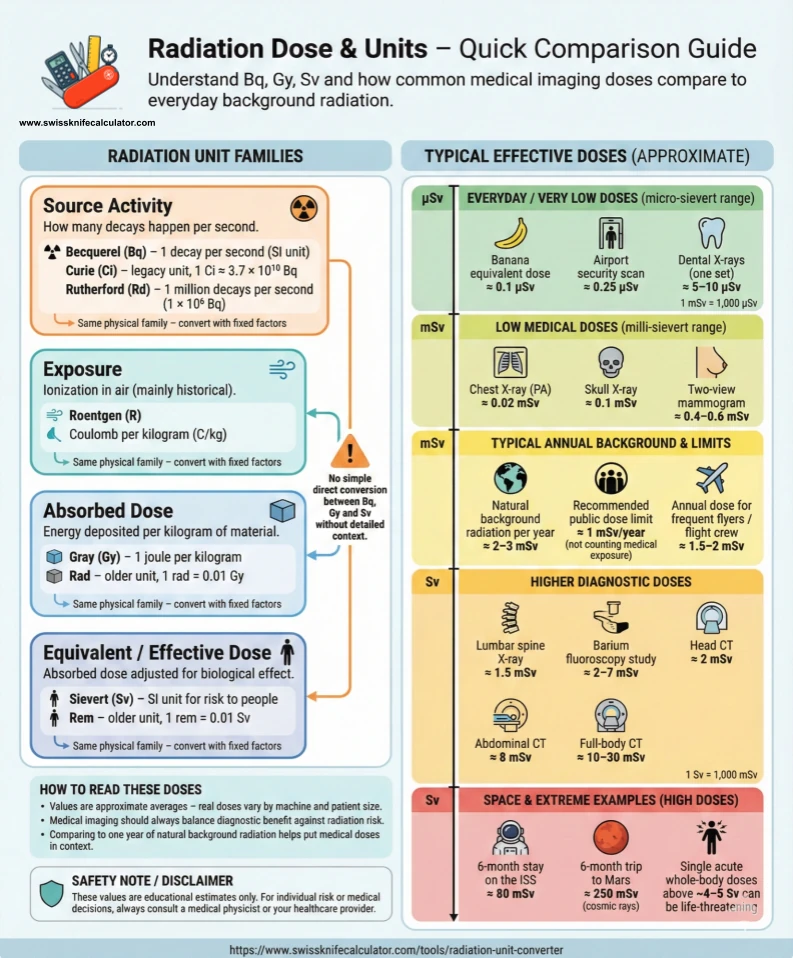
Use this infographic together with the Radiation Unit Converter results: after you convert a dose in mGy or mSv, you can quickly place it on the scale – for example, “this dose is similar to a chest X-ray” or “this is in the range of a single CT scan” – and compare it to annual background radiation.
FAQ
What is the difference between gray and sievert?
Gray (Gy) measures absorbed dose (energy per kg). Sievert (Sv) applies a weighting to estimate biological effect; for X-rays the factor is often 1, but it can differ for other radiation types.
Why use becquerel instead of curie?
Becquerel (Bq) is the SI unit for activity: 1 Bq = 1 decay per second. Curie is legacy: 1 Ci = 3.7×10^10 Bq.
Can I convert roentgen to sievert?
Not as a single universal factor. Roentgen (R) describes ionization in air, while sievert relates to dose in tissue; you need radiation energy/type and geometry to estimate Sv.
Is rad still used?
Yes in some older medical and nuclear documents. 1 rad = 0.01 Gy, so 100 rad = 1 Gy.
What does 1 mSv mean?
1 mSv is 0.001 Sv. It is a small equivalent/effective dose unit commonly used for imaging and background comparisons.
Are these conversions linear?
Within the same quantity family, yes (they are simple multipliers). Between different families (activity ↔ dose ↔ exposure), no—context is required.
What’s a quick CT dose range in mSv?
A typical CT effective dose is often a few mSv and can be around 2–10 mSv depending on scan type and protocol.
Why can’t I convert Bq to Gy directly?
Activity counts decays per second; absorbed dose depends on energy deposited in a mass over time. You need emission energies, exposure time, distance/shielding, and the material/tissue to estimate Gy.
How do I enter µSv or mGy if the dropdown shows Sv or Gy?
Use decimal scaling: 500 µSv = 0.0005 Sv and 2 mGy = 0.002 Gy. The conversion stays exact because the unit multipliers are linear.
What is MU and can it be converted to Gy?
MU (monitor unit) is a machine-specific linac output counter. Converting MU to dose requires your local calibration (for example cGy per MU) and reference conditions.
Important limits & disclaimer
- Educational only: no guarantees; not medical, legal, or regulatory advice.
- No cross-category conversion: activity ↔ dose ↔ exposure requires modeling assumptions and may be highly scenario-dependent.
- Context-sensitive values: effective-dose ranges vary by protocol, equipment, and patient factors.
- Clinical use: the MU helper is a conceptual check; treatment planning must use verified TPS/QA workflows.
